In the last 10 years a new form of cognitive behavioral therapy (CBT), called CBT-E (“enhanced” CBT) and derived from evidence-based CBT for bulimia nervosa has been developed by Christopher Fairburn and colleagues in Oxford (UK), with a view to treating the psychopathology behind the eating disorder, rather than the eating disorder itself. CBT-E can truly be described as ‘enhanced,’ not only because it uses a variety of new strategies and procedures to improve treatment outcomes in bulimia nervosa, but also because it lends itself to treating all recognized diagnostic categories of eating disorder (i.e., anorexia nervosa, bulimia nervosa, and eating disorder not otherwise specified – NOS) in an outpatient setting. Indeed, the first randomized controlled trial of this innovative approach showed that CBT-E is as effective for not significantly underweight eating disorder NOS patients as it is for patients with bulimia nervosa, with two-thirds of those who completed treatment showing a good outcome. Promising findings have also been reported from a three-site joint UK/Italian study of CBT-E treatment in adult outpatients with anorexia nervosa, by a an Italian study in adolescent patients with anorexia nervosa, and by an Australian effectiveness study that successfully used CBT-E to treat a transdiagnostic sample of patients with anorexia nervosa, bulimia nervosa and eating disorder NOS.
Having verified the effectiveness of CBT-E for the spectrum of eating disorders in our own clinic, my colleagues and I set out to adapt this original approach for more intensive levels of care. The rationale behind extending CBT-E to inpatient and intensive outpatient settings was based on three main considerations: first, some patients fail to respond to outpatient CBT-E altogether, and some have an eating disorder of such clinical severity that they cannot be managed safely in an outpatient setting; second, data on changing the type of outpatient treatment in patients who are not responding to CBT are inconclusive, but in these cases the alternative to outpatient treatment is generally hospitalization in specialized eating disorder units, which, unfortunately tend to adopt an eclectic approach not driven by a single theory of empirically supported efficacy; and third, the ineffectiveness of outpatient CBT-E in some patients may depend on insufficiently intensive care rather than the nature of the treatment itself.
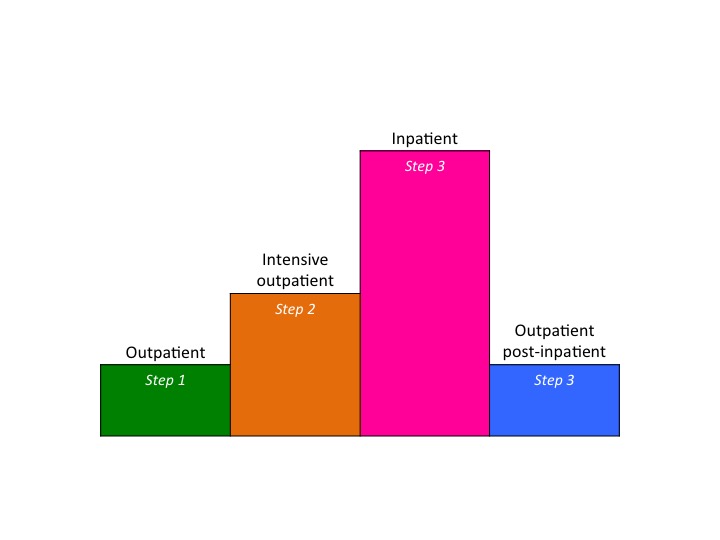
It follows then that the availability of a treatment able to address all the diagnostic categories of clinical eating disorders in different care settings (from outpatient to inpatient through intensive outpatient) is sorely needed. In this context, multistep CBT-E offers, for the first time in the field of evidence-based psychotherapy for eating disorders, the concrete possibility of implementing such a treatment within a stepped-care approach in real world clinical settings. Indeed, the most distinctive and unique characteristic of multistep CBT-E, and perhaps the most significant, is that the same theory and procedures are applied at each level of care. The only difference between the various steps is the intensiveness of treatment, with less unwell patients being treated using outpatient CBT-E procedures, and the more severely affected sufferers being channeled directly to inpatient CBT-E. Within this three-step approach, non-responders to outpatient treatment, and those who would benefit from more support but whose physical conditions do not warrant hospitalization, can be offered a more intensive form of outpatient treatment within the CBT-E framework (Figure 1). Thus, patients can be moved seamlessly from outpatient to inpatient care, and then on to the final phase of outpatient treatment, with no change in the nature of the treatment itself. It is hoped that this “standardization” of approach will improve the chances for recovery in these patients, as it would avoid subjecting them to confusing and counterproductive changes in therapeutic approach that commonly accompany such transitions.
The validity of this hope is supported by a recent Italian study, which tested the effectiveness of CBT-E, previously only trialed in outpatients, in a group of 80 hospitalized patients with severe anorexia nervosa. The results showed that the treatment produced a substantial improvement in weight, eating disorder features and general psychopathology in these patients, and attenuated the weight loss that typically follows hospitalization for anorexia nervosa.
Figure 1. Multistep CBT-E. Every level of care is based on the same theory, and uses similar strategies and strategies (more intensive in intensive outpatient and inpatient CBT-E)
References
Dalle Grave R. A multi-step cognitive behaviour therapy for eating disorders. European Eating Disorders Review 2005;13:373-82.
Dalle Grave, R. (2013). Multistep Cognitive Behavioral Therapy for Eating Disorders: Theory, Practice, and Clinical Case. Lanham: Jason Aroson (tr. it Terapia Cognitivo Comportamentale Multistep per i Disturbi dell’Alimentazione. Teoria, Pratica e Casi Clinici. Eclipsi: Firenze, in press).
Dalle Grave, R. (2012). Intensive Cognitive Behavior Therapy for Eating Disorder. Hauppauge NY, Nova Publisher.
Dalle Grave R, Calugi S, El Ghoch M, Conti M, Fairburn CG. Inpatient cognitive behavior therapy for adolescents with anorexia nervosa: Immediate and longer-term effects. Frontiers in Psychiatry 2014; 5: 1-6.
Dalle Grave, R., Calugi, S., Doll, H. A., & Fairburn, C. G. Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: an alternative to family therapy? Behaviour Research and Therapy 2013; 51: R9-R12.
Dalle Grave R, Calugi S, Conti M, Doll HA, Fairburn CG. Inpatient cognitive behaviour therapy for anorexia nervosa: A randomized controlled trial. Psychotherapy and Psychosomatics 2013; 82: 390-398.
Fairburn CG. Cognitive Behaviour Therapy and Eating Disorders. Guilford Press, New York, 2008 (tr it. Terapia Cognitivo Comportamentale dei Disturbi dell’Alimentazione. Eclipisi: Firenze, 2010)
Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy 2003:509 – 28
Fairburn C.G, Cooper Z, Doll HA, Palmer RL, Dalle Grave, R. Enhanced cognitive behaviour therapy for adults with anorexia nervosa: a UK-Italy study. Behaviour Research and Therapy 2013; 51: R2-R8.
Fairburn, C. G, Cooper, Z, Doll, H. A., O’Connor, ME, Bohn, K, Hawker, DM, . . . Palmer, RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: A two-site trial with 60-week follow-up. American Journal of Psychiatry 2009; 166: 311-319.
Poulsen S, Lunn S, Daniel SIF, Folke S, Mathiesen BB, Katznelson H, Fairburn CG. A randomized controlled trial of psychoanalytic psychotherapy versus cognitive behavior therapy for bulimia nervosa. American Journal of Psychiatry 2014; 171: 109-116.